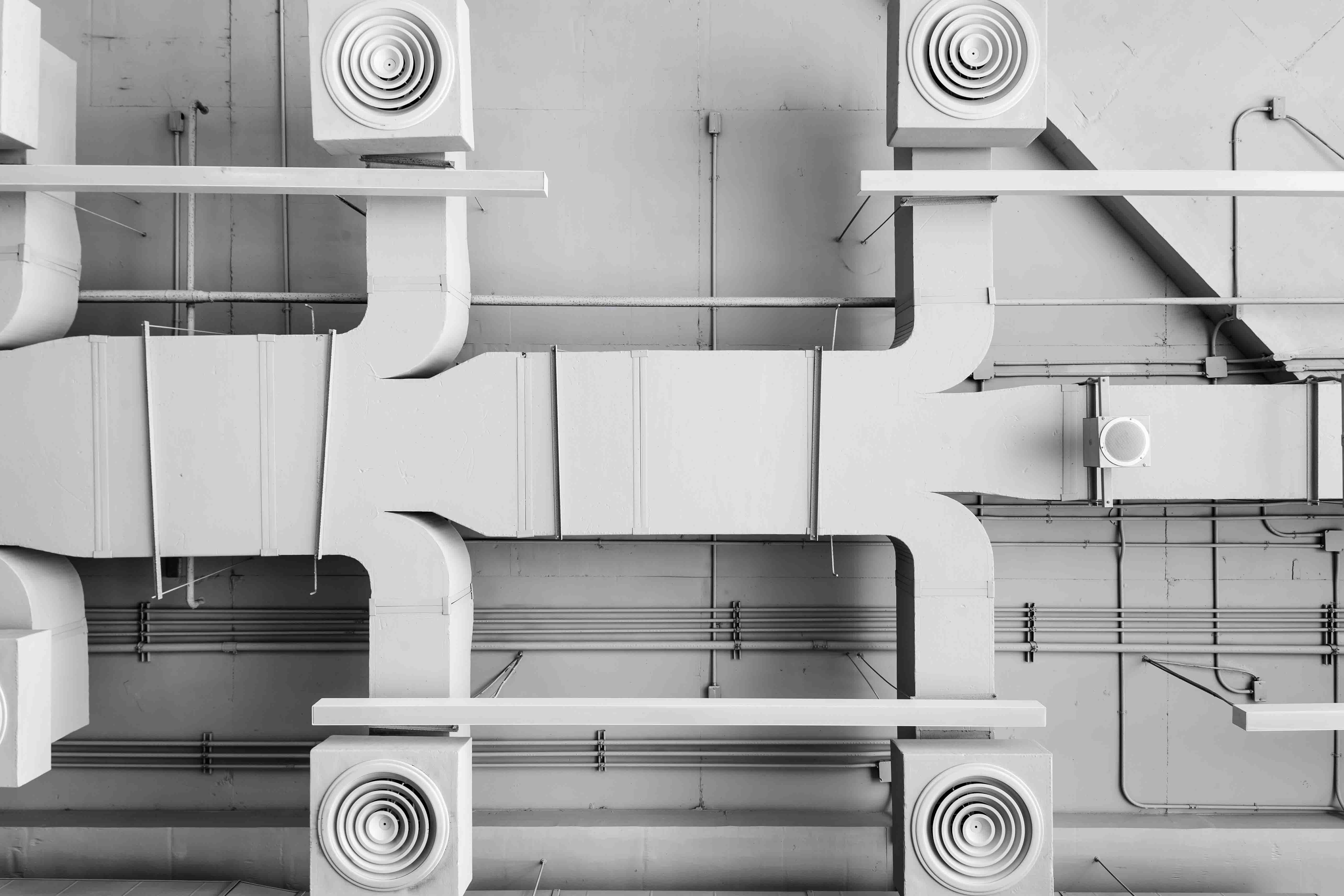
HVAC Strategies to Control Airborne Pathogens
By Grainger Editorial Staff 6/9/20
Influenza, COVID-19 and other viral respiratory illnesses can spread from one person to another via airborne pathogens. People who are infected may expel pathogenic material into the air by coughing, sneezing, talking or even just by breathing.
Controlling the spread of infection in a facility is absolutely critical during a pandemic, and highly desirable at all times. Facility managers and engineers can help control airborne pathogens by modifying the HVAC operations in their facilities. Building technology organization ASHRAE has published a document on infectious aerosols describing evidence-based HVAC strategies that can help lower the risk of infection. The Environmental Protection Agency (EPA) has referred building professionals to ASHRAE resources for guidance on how HVAC operations can address COVID-19.
Droplets and Aerosols: What's the Difference?
To understand how HVAC operations can influence airborne pathogens, it's important to know that infectious material is carried through the air by particles that behave differently depending on their size.
Some infectious material is carried by larger droplets, such as those produced by sneezing or coughing. (Thus the importance of social distancing and cloth face coverings.) Most large droplets settle rapidly onto surfaces fairly close to their source—about three to seven feet away, according to ASHRAE. The organization states that HVAC systems don't have much influence on the behavior of larger droplets that transmit illness over short distances.
But pathogenic material is also carried by smaller droplets that can be aerosolized. This means that they're suspended in the air, much like a mist, remaining aloft for minutes, hours or even days depending on the particle size, and capable of traveling long distances under the right conditions. According to one study, people infected by influenza may produce pathogenic aerosols without sneezing or coughing—simply by breathing.
HVAC systems can play a role in controlling the movement of infectious aerosols, helping to dilute them, to conduct them out of occupied spaces and to eliminate them through filtration—thus helping prevent the spread of airborne illness within the facility.
Planning for Pandemic Response
During pandemics and other emergencies, the following modifications to HVAC operations may help decrease exposures to airborne pathogens, according to ASHRAE. The organization suggests considering these options for inclusion in emergency response plans in non-healthcare buildings.
Increase Outdoor Air Ventilation
- Disable demand control ventilation (DCV) systems, which are designed to reduce ventilation when there are fewer people in a space than its designed occupancy.
- Open outdoor air dampers to 100%. Outdoor air dampers control the flow of fresh air into a building and are normally integrated into a building's air-handling system. In older buildings they may be manually operated, while in newer buildings they may be part of an economizer that draws fresh air into a building as an energy-saving measure under certain conditions.
Install Higher MERV Filters
- Improve air filtration to MERV-13, if possible. HVAC filters have a minimum efficiency reporting value (MERV) that indicates the smallest particles that the filter can effectively remove. Filters that trap smaller particles have higher MERV ratings. High MERV ratings may be difficult to attain in some systems because they can lead to pressure drop, which can potentially reduce airflow and diminish the system's ability to maintain humidity and temperature set points.
Keep HVAC Systems Running
- Leave HVAC systems running as long as possible in emergency situations, up to 24/7 if possible. No matter what level of filtration your system has, it can only remove particles when the fan is running.
Use Portable Room Air Cleaners
- Portable air cleaners (also called air purifiers and air scrubbers) with HEPA filters or high MERV filters are designed to clean the air in a single room or area. Learn more in our complete air purifier guide.
- In residential settings, the EPA advises placing the devices so that the air they filter reaches people's breathing space as directly as possible, without being obstructed by furniture or encountering sources of small particles such as printers.
Use UVGI Devices
- Ultraviolet germicidal irradiation (UVGI), also called ultraviolet germicidal energy, is a technology that uses light as a disinfectant. The entire UV spectrum can kill or inactivate microorganisms, but UVC energy provides the most germicidal effect. Most contemporary UVGI lamps produce UVC energy at near-optimum wavelengths. This energy damages the nucleic acids and proteins of pathogens, making them inactive and unable to transmit infection.
- Consider UVGI devices for high-density locations such as waiting rooms. Some UVGI units can be mounted in ducts or air-handling units. There are also upper-room UVGI units that can be effective particularly with fans. Portable UVGI devices are also available
- For more information on designing and implementing systems, see the CDC guidance on upper-room UVGI strategies.
Control the Humidity
- There is evidence that controlling relative humidity can reduce transmission of some airborne pathogens. According to ASHRAE, midrange humidity levels are associated with improved immunity against respiratory infections. While ASHRAE does not recommend a specific humidity target, the organization notes that relative humidity below 40% is associated with a number of factors that increase infections. A research review published in the Annual Review of Virology stated that the ideal relative humidity for preventing aerosol transmission of respiratory viruses is between 40% and 60%.
- When using a humidifier to maintain midrange humidity in cold climates, facility managers should beware of thermal bridges, according to ASHRAE. A thermal bridge is a place where improper insulation allows heat to rapidly escape the building in cold weather. This can lead to condensation and eventually mold growth. The humidifiers themselves should also be cleaned and treated to prevent the growth of mold or bacteria.
Bypass Energy Recovery Ventilation Systems
- Energy recovery ventilators (ERVs) use an HVAC system's exhaust air to pretreat outside air as it comes in. One popular ERV design uses a rotary heat exchanger—a plastic or metal wheel—that transfers heat from one stream to the other as it rotates. While ERVs save energy, some designs may allow leakage of air from the exhaust stream to the incoming stream. ASHRAE standards permit some leakage to occur, depending on the kind of air being exhausted, but in pandemics and other emergencies it may be desirable to eliminate as much of this leakage as possible.
Preparing Building Automation Systems
- Consider programming building automation system control sequences that consolidate infection-mitigating HVAC strategies into emergency response modes that that can be applied by the operator with one press of a button.
Reopening a Facility
- In addition to the emergency planning recommendation in ASHRAE's document on infectious aerosols, the organization has published guidance for restarting operations in buildings that were closed during the COVID-19 pandemic. See the full list under "How to Return the HVAC System to Normal Operations FAQ" on ASHRAE's COVID-19 frequently asked questions page.
Airflow Patterns and Other Design Considerations for the New Normal
The HVAC modifications described above are intended to be considered as part of an emergency response plan in non-healthcare facilities. Along with these emergency measures, ASHRAE also lists HVAC strategies to consider implementing for normal, non-emergency operations, based on a hazard assessment.
These non-emergency strategies echo many of ASHRAE's proposed emergency measures and include:
- Higher MERV filters
- Portable air cleaners
- Upper-room UVGI (upper-room installation helps maintain safe levels of UVGI in the occupied, lower portion of the room, according to guidance from the CDC)
- Humidity/temperature control
Additionally, ASHRAE recommends designing ventilation systems to promote clean airflow patterns, allowing airborne particles to leave the space. While the organization has not published detailed documentation on how to achieve this in non-healthcare facilities, they have collected guidance and resources that cover airflow patterns in healthcare environments and other topics.
HVAC Design Strategies for Healthcare Facilities
ASHRAE recommends that healthcare facilities consider the following HVAC strategies:
- Maintain negative pressure in rooms where there may be infectious aerosols, which may include intensive care units (ICUs).
- Exhaust toilets and bedpans (in other words, restrooms and bedpan closets)—ASHRAE describes this as "a must"
- Provide 100% exhaust in patient rooms.
- Increase the outdoor air change rate, measured in air changes per hour (ACH). For example, consider increasing the hourly changes of outdoor air in patient rooms from the CDC-recommended minimum of two ACH to six ACH.
- Capture potentially infectious aerosols with headwall exhaust; tents or snorkels with exhaust; floor-to-ceiling partitions with door supply and patient exhaust; and HEPA-grade filtration of local air.
- Deliver clean air to workers and caregivers.
- Maintain temperature and humidity "as applicable to the infectious aerosol of concern."
- Use UVGI air disinfection.
- When planning patient room turnover, consider the HVAC contribution.
- Design airborne infection isolation rooms (AIIRs) to include anterooms.
Commonly Asked Questions
Q: Should HVAC systems be turned off to reduce the risk of COVID-19 transmission?
A: ASHRAE states that in general disabling HVAC systems is not recommended as method to reduce transmission of the virus that causes COVID-19. It is the organization's view that HVAC systems can lower the concentration of viral material in the air and thus lower the risk of transmission, and that people in unconditioned environments may be subjected to unhealthy temperature stress.
Q: How does relative humidity in a building effect transmission of infection?
A: According to research summarized by ASHRAE, there are three ways that low humidity can makes transmission of respiratory infections more likely. While this research is not specific to COVID-19, it is applicable to respiratory infections in general. First, large infectious particles can shrink in dry air to become droplet nuclei, which are dormant but still infectious and can travel long distances. Second, many viruses are most viable in low humidity. Third, there is evidence that ambient humidity below 40% lowers immune system defenses, in part by impairing mucus membrane barriers. Detailed analysis of many of these issues can be found in "Seasonality of Respiratory Infections."
Q: Can HVAC filtration help prevent the spread of illness?
A: There is evidence that filtration can help remove infectious aerosols, according to ASHRAE. The organization suggests that upgrading HVAC filtration to MERV-13 (or the highest level achievable in the system) can be a useful step in pandemic response plans.
Q: What is a respiratory droplet?
A: People produce respiratory droplets when they cough, sneeze, talk and breathe. These droplets are composed mostly of water but can also include cells from the person who emitted them, eloctrolytes from that person's mucous or saliva, and infectious agents such as viruses and bacteria, according to research published by the World Health Organization. The smallest droplets can remain suspended in air for long periods of time, while larger droplets fall quickly to the ground.
The information contained in this article is intended for general information purposes only and is based on information available as of the initial date of publication. No representation is made that the information or references are complete or remain current. This article is not a substitute for review of current applicable government regulations, industry standards, or other standards specific to your business and/or activities and should not be construed as legal advice or opinion. Readers with specific questions should refer to the applicable standards or consult with an attorney.











